ABSTRACT
OBJECTIVE: To describe mortality due to hepatitis B and C as underlying cause in the municipality of São Paulo, verifying the trend of these rates, and to assess the association of these diseases with others, from 2002 to 2016.
METHODS: This is a time series study on mortality due to hepatitis B and C according to sex, with data from the Sistema de Informação de Mortalidade (SIM – Mortality Information Sistem). Prais Winsten regression was used in rate trend analysis.
RESULTS: The findings of this study showed a trend of decline of mortality from hepatitis B and C in recent years, particularly among males. These infections were important associated causes of liver cell carcinoma and HIV. The proportion of deaths under 70 years of age stands out.
CONCLUSIONS: The study provides a baseline for research on mortality trend and the impact of interventions, given the history of expanded detection and supply of treatments, including the most recent antivirals in Brazil, since 2015.
DESCRIPTORS: Hepatitis B; Hepatitis C; Mortality, trends; Time Series Studies
RESUMO
OBJETIVO: Descrever a mortalidade por hepatites B e C como causa básica no município de São Paulo, verificando a tendência dessas taxas, e avaliar a associação dessas doenças a outras no período de 2002 a 2016.
MÉTODOS: Trata-se de um estudo de série temporal sobre mortalidade por hepatites B e C segundo sexo, com dados do Sistema de Informação de Mortalidade. A regressão de Prais Winsten foi usada na análise de tendência das taxas.
RESULTADOS: Os achados do presente estudo mostraram tendência de declínio da mortalidade por hepatites B e C nos últimos anos, particularmente entre pessoas do sexo masculino. Essas infecções foram causas associadas importantes ao carcinoma de células hepáticas e ao HIV. Destaca-se a proporção de óbitos com menos de 70 anos de idade.
CONCLUSÕES: O estudo fornece uma linha de base para pesquisas de tendência de mortalidade e de impacto de intervenções, visto o histórico de ampliação da detecção e oferta de tratamentos, incluindo os mais recentes antivirais no Brasil, desde 2015.
DESCRITORES: Hepatite B; Hepatite C; Mortalidade, tendências; Estudos de Séries Temporais
INTRODUCTION
Hepatitis B and C have great magnitude in the world, with estimates of about 257 million people chronically infected by the first (HBV) and 71 million by the second (HCV)1. In Brazil, a population survey performed in the Brazilian capitals and the Federal District in the 2010s showed prevalence of 0.37% and 7.40% for the surface antigen of virus B (HBsAg) and against its nucleus (Anti-HBc), respectively, and 1.38 for the antibody against virus C (Anti-HCV)2–4. This resulted in an estimate for the population inhabiting these areas of 430,658 of people with Anti-HCV reactivity, being 36.70% viremic4. In 2016, the Brazilian Ministry of Health estimated a prevalence of 0.70% nationwide and of 657,000 people with the active hepatitis C virus, aiming to establish a baseline to estimate the cases to be diagnosed and treated annually, in order to meet targets and eliminate viral hepatitis by 20305. In a more recent publication, these estimates were updated to 0.53% and 632,000, respectively6. This information shows the importance of these infections in Brazil and the challenge for health services in detecting and treating patients.
Chronic HBV or HCV has been associated with an increased risk of death, especially from causes related to the development of liver diseases, such as cirrhosis or hepatocellular carcinoma (HCC). In 2015, 887,000 people died as a result of HBV infection7, and, in 2016, approximately 399,000 die each year with hepatitis C, mainly from cirrhosis and hepatocellular carcinoma8.
Viral hepatitis is among the main causes of death worldwide, being HCC the only cancer that substantially increased between 1990 and 20139. In Brazil, the mortality rate from hepatitis B from 2000 to 2009 was 0.3/100,000 inhabitants-year10.
It should be noted that studies on hepatitis C mortality are scarce5. In the municipality of São Paulo, the mortality trend due to hepatitis B or C has not yet been evaluated. Thus, the objective of this study was to describe mortality due to hepatitis B and C as underlying cause in the city of São Paulo, verifying the trend of these rates, and to evaluate the participation of these infections as causes associated with others from 2002 to 2016.
METHODS
This is an ecological time series on mortality from viral hepatitis B and C, from 2002 to 2016, including deaths of residents in the city of São Paulo.
The São Paulo capital has a territorial area of 1,522,986 km2, an estimated population of 11,638,802 inhabitants11 in 2016, and Municipal Human Development Index of 0.80512.
We used data on deaths in the municipality from 2002 to 2016, recorded in the Sistema de Informações sobre Mortalidade (SIM – Mortality Information System)13. The data source was the Programa de Aprimoramento das Informações de Mortalidade (PRO-AIM – Mortality Information Improvement Program), municipal administrator of the SIM and responsible for feeding information, sending it to the federal base and maintaining the municipal system. PRO-AIM has methods to improve the information contained in death certificates, in order to achieve and maintain a good quality of the system, such as sending letters to certifying doctors for clarification of doubts, investigation with the Instituto Médico Legal and the Serviço de Verificação de Óbitos, among others14. To estimate the rates, we used population estimates of the Fundação Sistema Estadual de Análise de Dados (SEADE)11.
Death from chronic hepatitis B was defined as those with the following codes from the International Classification of Diseases (ICD-10)15: B16.0 [acute hepatitis B with Delta-agent (co-infection) with hepatic coma], B16.1 [acute hepatitis B with Delta-agent (co-infection) without hepatic coma], B16.2 [acute hepatitis B without Delta-agent with hepatic coma], B16.9 [acute hepatitis B without Delta-agent and without hepatic coma], B17,0 [acute delta-super infection of hepatitis B carrier], B18.0 [chronic viral hepatitis B with Delta-agent] and B18.1 [chronic viral hepatitis B without Delta-agent] The definition of death from hepatitis C included ICD-10 codes B17.1 [acute hepatitis C] or B18.2 [chronic viral hepatitis C]16.
The underlying cause of death is defined by the World Health Organization as “(a) the disease or injury which initiated the train of morbid events leading directly to death, or (b) the circumstances of the accident or violence which produced the fatal injury.” Associated causes are all those described in the death certificate different from the underlying cause, that is, conditions that contributed to the death process (contributors) or that were complications of the underlying cause (consequential). All those described in the death certificate constitute multiple causes, that is, the underlying and associated causes15,16.
Initially, we only considered deaths with hepatitis B or C as underlying cause, to estimate the mortality rates and for trend analysis. Then, we analyzed the frequency with which hepatitis B or C were associated with deaths that had other underlying causes. For this, the associated causes for defining death were verified, that is, we considered the presence of the ICD-10 codes15 previously mentioned in any line of the death certificate17.
The gross mortality rate was estimated as the coefficient between total of deaths attributed to hepatitis B or C and the population in the studied age group residing in the municipality of São Paulo and multiplied by 100,000. The mortality coefficients were standardized by the direct method, using as reference the population of the 2010 census of the municipality of São Paulo.
The trend analysis was performed using a linear regression model for time series with the Prais-Winsten method, in order to minimize the first-order autocorrection of residues. The dependent variables were the standardized mortality rates from hepatitis B and C, and the independent variable was the calendar year18. We used the software Stata, version 15, for the statistical analysis of the data.
The project was approved by the Ethics Committee of the Municipal Health Secretariat of the city of São Paulo (Opinion No. 510.009, February 6, 2014).
RESULTS
Hepatitis B
From 2002 to 2016, 1,243 deaths were recorded in the SIM in the city of São Paulo mentioning viral hepatitis B, being 540 (43.44%) coded as underlying cause and 703 (56.55%) as associated cause.
Among the 540 deaths with hepatitis B as underlying cause, 127 (23.52%) were due to acute infection and 413 (76.48%) due to chronic infection. Among the patients, 69.60% were male and 30.40% were female. The predominant race/color was white (61.11%), and the majority (61.65%) had less than 8 years of schooling. The mean age of females was 66.00 years, higher than that of males (58.61 years). About two thirds of deaths were of people under 70 years of age, and this percentage is higher in males, with 75.83% (Table 1). No deaths of people under 15 years of age were recorded.
Characteristics of deaths due to hepatitis B and C as underlying causes, São Paulo, SP, 2002–2016.
As for the associated causes, we found 289 (53.52%) deaths with liver cirrhosis and 22 (4.07%) with hepatocellular carcinoma (data not shown in tables).
From 2002 to 2016, mortality rates from hepatitis B as underlying cause varied from 0.17 (2003 and 2006) to 0.58 (2013) per 100,000 inhabitants-year. There was an annual decline of 5.10% (95%CI: −8.26; −1.82%) in males (-4.75%; 95%CI: −7.03; −2.42%), but not in females (-6.79%; 95%CI: −14.10; 1.14%) (Figure 1 and Table 2).
Standardized mortality rates for hepatitis B as underlying cause, according to sex and year of death, São Paulo, SP, 2002–2016.
Mean annual variation in mortality rates from hepatitis B and C as underlying causes, according to sex and study period, São Paulo, 2002–2016.
Hepatitis B was mentioned in 703 deaths whose underlying cause were diseases constant in ICD-10 chapters. The highest proportion is associated with diseases from Chapter II, referring to neoplasms (C00-D48), with 42.53% of deaths (n = 299), and Chapter I, referring to infectious and parasitic diseases (A00-B99), with 30.44% (n = 214). Among neoplasms, liver cell carcinoma (C22.0) (56.18%, 169/299) and unspecified malignant liver neoplasm (C22.9) stand out, with 57 deaths (19.06%, 57/299). Among infectious diseases, those associated with HIV stand out (B20.0, B20.1, B20.3, B20.6, B20.7, B20.8, B21.0, B22.7, B24), with 172 deaths (80.37%, 172/214). Among these, 14 deaths also stand out, in which the underlying cause was hepatitis C (B17.1 and B18.2) (6.54%, 14/214). In Chapter XI – Diseases of the Digestive System, 28 deaths due to diseases related to alcohol intake are noticeable (K70.0, K70.1, K70.3, K70.4 and K70.9) (data not shown in tables).
Hepatitis C
From 2002 to 2016, 6,419 deaths were recorded with mention to hepatitis C, being 3,194 (49.76%) as underlying cause and 3,225 (50.24%) as an associated cause in residents of the city of São Paulo.
Among the 3,194 people who died with hepatitis C as underlying cause, 55.10% were males and 44.90% females. The race/color white was in 76.02% of the records, and 48,90% of the patients had less than 8 years of schooling. Mean age was 61.72 years, greater among women (65.64 years) compared with men (58.51 years). There were no records of deaths in children under 15 years of age. It was found that 72.12% of the deaths were of people under 70 years of age, being this percentage higher in males, with 81.91% (Table 1).
In addition, 1,801 deaths (56.41%) from hepatitis C also had hepatic cirrhosis as associated cause. Of these cases, women (44.50%) had a mean age of 66.22 years, and men (55.50%), 57.93 years. We identified 196 (6,14%) deaths with hepatocellular carcinoma as associated cause (data not shown in tables).
The mortality rates from hepatitis C as underlying cause showed an increase of 5.65% per year (95%CI 2.99; 8.39%) between 2002 (1.99/100,000 inhabitants-year) and 2009 (3.07/100,000 inhabitants-year), both in males (4.60%; 95%CI 2.41;6.84%) and females (6.90%; 95%CI 3.03;10.91%). From 2009 to 2016, there was an annual decrease trend of 4.79% (95%CI −7.44; −2.07), decreasing to 1.98/100,000 inhabitants in 2016. This decline was found in males (-4.95%; 95%CI −7.63; −2.19%), but not in females (-5.29%; 95%CI −10.98; 0.76%) (Figure 2 and Table 2).
Standardized mortality rates for hepatitis C as underlying cause, according to sex and year of death, São Paulo, SP, 2002–2016.
In relation to the 3,225 deaths mentioning hepatitis C as associated cause, the greater proportion has neoplasms as underlying cause (Chapter II of ICD-10, C00-D48, n = 1,246, 38.63%), followed by infectious and parasitic diseases (Chapter I of ICD-10, A00-B99, n = 893, 27.69%). Among the neoplasms, liver cell carcinoma (C22.0) accounted for 59.95% of deaths (747/1,246), followed by unspecified malignant liver neoplasm (C22.9) (14.77%, 184/1,246). Among infectious diseases, 78.61% of deaths (702/893) had diseases associated to HIV as underlying cause (B20.0, B20.1, B20.2, B20.3, B20.6, B20.7, B20.8, B21.0, B21.1, B21.7, B21.8, B22.0, B22.7, B23.2, B24), and 7.61% (68/893) had hepatitis B (B16.2, B16.9, B18.1). It is worth noting that 113 individuals died of liver diseases related to alcohol intake (K70.0, K70.1, K70.3, K70.4 and K70.9) (data not shown in tables).
DISCUSSION
The findings of this study showed a trend of declined mortality from hepatitis B and C in recent years in the municipality of São Paulo, particularly in males. These infections were important causes associated to liver cell carcinoma and HIV. In addition, the proportion of individuals who died under 70 years of age stands out (about 70%).
The analysis of mortality trend from hepatitis B showed reduction, particularly in men. In the USA, the mortality trend from hepatitis B between 1999 and 2007 showed that the annual age-adjusted mean was relatively constant19. But, in other places, such as Taiwan, a hyper-endemic region in past decades, there has been sharp decreases4,20,21. We suggest that the decreased mortality rates from hepatitis B in Brazil may be attributed in part to vaccination, with decreased prevalence, but also to prevention measures against infections by HIV initiated in the 1980s, as observed in other countries4,22,23.
In relation to mortality from hepatitis C, there was a mean increase trend of 5.65% per year between 2002 and 2009, in both sexes, and reduction of 4.79% from 2009 to 2016, in males. In the US, the standardized annual mortality rate increased and exceeded AIDS mortality between 1999 and 200719. In Brazil, the percentage drop in the second period stands out, which may be, in part, due to the treatment instituted in the Country at the beginning of the previous decade, with double therapy, used until 2014, including pegylated interferon as one of its components, in addition to the increased uptake of infected people by health services24–26. In 2015, the Ministry of Health instituted the treatment with new direct-acting antivirals, which show efficacy of more than 90% in curing hepatitis C and lower rates of adverse effects27.
Clinical care for the patient with HCV has advanced considerably, due to the evolution of diagnostic procedures and the improvement in therapy and prevention. The treatment of the infection has been proposed and improved for about 20 years, with a therapeutic arsenal of progressively better efficacy.
In many countries, the incidence of hepatitis B and C has decreased due to fewer new infections. However, the prevalence of severe liver diseases continues to increase, since there is a contingent of people infected with HBV and HCV in past decades who are unaware of their condition or who were diagnosed late, when they show signs and symptoms of severe liver disease, such as cirrhosis and HCC, which contributes to premature death9,28.
In the US, a cohort study, from 2006 to 2010, showed mean age of 57 years for deaths from hepatitis C29. Another study conducted in the city of New York, with a casuistry from 2000 to 2011, pointed out that 64.10% of the deaths of individuals infected by HCV occurred before 65 years of age30.
In this study, it was observed that at least two thirds of deaths from hepatitis B and C affected individuals under the age of 70, that is, those born between 1945 and 1965 (“baby boomers”). In the case of hepatitis C, these people became infected mainly before the incorporation of screening in blood banks and new technologies of products and processes related to the control of blood and blood products, as well as biosecurity standards in health services31. This finding strengthens the recommendation for Anti-HCV testing in people born in this period, since the infection may be asymptomatic in 75% of the cases32, as well as for instituting early treatment and vaccination against HBV in these carriers, according to the recommended protocol, preventing the aggravation of their condition33.
The significant proportion of hepatitis B and C contributing as causes associated with HCC and HIV is consistent in other findings in literature. A systematic review of studies published in several countries showed that chronic viral hepatitis due to HBV and HCV contribute to the majority of HCC occurences33. Globally, 78% of HCC infections were attributed to HBV (53%) and HCV (25%), confirming that chronic hepatitis B and C represent the main cause of primary liver cancer in the world7–8,33. The co-infection of viral hepatitis with HIV may be explained by the common routes of infection, mainly parenteral and sexual34, and is associated with a higher risk of death27,35. Progression from liver fibrosis to cirrhosis is accelerated in individuals with concomitant hepatitis C and HIV36.
Mortality data from this study may be underestimated due to the absence of hepatitis B and C in the death certificate, either as underlying or associated cause28. The associated causes of death were also studied to try to understand the effect of the under-registration of hepatitis B and C as underlying cause, especially when associated with liver cirrhosis, HCC and HIV infection37.
Mortality statistics according to underlying cause no longer show the total impact of a disease or aggravation in a set of deaths38. This study enabled this broader and more complete view, evidencing the presence of viral hepatitis B and C as associated causes, in order to contribute to the knowledge of the epidemiological profile of these diseases in our environment.
The data found show the importance of prevention and early diagnosis and treatment of hepatitis B and C. The contribution of this study is to provide a baseline for new studies on mortality trend and evaluation of the impact of new interventions, considering the expansion of diagnosis and treatment offer, including the most recent antivirals in Brazil, since 201527, regardless of the degree of liver fibrosis, since 201939. In addition, these results may support the achievement of predicted goals for eliminating hepatitis B and C in the city of São Paulo39,40.
REFERENCES
- 1 World Health Organization. Prevention and control of viral hepatitis infection: framework for global action. Geneva: WHO; 2012.
-
2 Pereira LMMB, Martelli CMT, Méchan-Hamann E, Montarroyos UR, Braga MC, Lima MLC, et al. Population-based multicentric survey of hepatitis B infection and risk factor differences among three regions in Brazil. Am J Trop Med Hyg. 2009;81(2):240-7. https://doi.org/10.4269/ajtmh.2009.81.240
» https://doi.org/10.4269/ajtmh.2009.81.240 -
3 Pereira LMMB, Martelli CMT, Moreira RC, Merchan-Hamman E, Stein AT, Cardoso MRA, et al. Prevalence and risk factors of Hepatitis C virus infection in Brazil, 2005 through 2009: a cross-sectional study. BMC Infect Dis. 2013;13:60. https://doi.org/10.1186/1471-2334-13-60
» https://doi.org/10.1186/1471-2334-13-60 -
4 Ximenes RAA, Figueiredo GM, Cardoso MRA, Stein AT, Moreira RC, Coral G, et al. Population-based multicentric survey of Hepatitis B infection and risk factors in the north, south, and southeast regions of Brazil, 10-20 years after the beginning of vaccination. Am J Trop Med Hyg. 2015;93(6):1341-8. https://doi.org/10.4269/ajtmh.15-0216
» https://doi.org/10.4269/ajtmh.15-0216 - 5 Ministério da Saúde (BR), Secretaria de Vigilância em Saúde, Departamento de DST/aids e Hepatites Virais. Plano para Eliminação da Hepatite C no Brasil. Brasília, DF; 2019.
-
6 Benzaken AS, Girade R, Catapan E, Pereira GFM, Almeida EC, Vivaldini S, et al. Hepatitis C disease burden and strategies for elimination by 2030 in Brazil. A mathematical modeling approach. Braz J Infect Dis. 2019;23(3):182-90. https://doi.org/10.1016/j.bjid.2019.04.010
» https://doi.org/10.1016/j.bjid.2019.04.010 -
7 World Health Organization. Hepatitis B. Geneva: WHO; 2020 [cited 2020 Sep 9]. Available from: https://www.who.int/news-room/fact-sheets/detail/hepatitis-b
» https://www.who.int/news-room/fact-sheets/detail/hepatitis-b -
8 World Health Organization. Hepatitis C. WHO; Geneva; WHO; 2020 [cited 2020 Sep 9]. Available from: https://www.who.int/news-room/fact-sheets/detail/hepatitis-c
» https://www.who.int/news-room/fact-sheets/detail/hepatitis-c -
9 GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151-1210. https://doi.org/10.1016/S0140-6736(17)32152-9
» https://doi.org/10.1016/S0140-6736(17)32152-9 -
10 Tauil MC, Amorim TR, Pereira GFM, Araújo WN. Mortalidade por hepatite viral B no Brasil, 2000-2009. Cad Saude Publica. 2012;28(3):472-8. https://doi.org/10.1590/S0102-311X2012000300007
» https://doi.org/10.1590/S0102-311X2012000300007 -
11 Fundação SEADE. Informações dos Municípios Paulistas. São Paulo; 2019 [cited 2019 Nov 1]. Available from: http://www.imp.seade.gov.br/frontend/#/
» http://www.imp.seade.gov.br/frontend/#/ -
12 Instituto Brasileiro de Geografia e Estatística. Índice de Desenvolvimento Humano Municipal – 2010. Rio de Janeiro: IBGE; 2010 [cited 2019 Nov 18]. Available from: https://cidades.ibge.gov.br/brasil/sp/sao-paulo/panorama
» https://cidades.ibge.gov.br/brasil/sp/sao-paulo/panorama -
13 Ministério da Saúde (BR). DATASUS. Arquivo de dados do Sistema de Informação de Mortalidade do Estado de São Paulo do período de 2002 a 2016. Brasília, DF; 2019 [cited 2019 Nov 1]. Avaliable from: http://www2.datasus.gov.br/DATASUS/index.php?area=0901&item=1&acao=26
» http://www2.datasus.gov.br/DATASUS/index.php?area=0901&item=1&acao=26 - 14 Prefeitura Municipal de São Paulo. Programa de Aprimoramento das Informações de Mortalidade. Coletânea de Textos dos boletins do PRO-AIM. São Paulo; 2003.
- 15 Organização Mundial da Saúde. CID-10. Classificação estatística internacional de doenças e problemas relacionados à saúde. 2.ed. São Paulo: Editora da Universidade de São Paulo;1997. v.1.
- 16 Laurenti R, Mello Jorge MHP. Atestado de óbito: aspectos médicos, estatísticos, éticos e jurídicos. São Paulo: Conselho Regional de Medicina do Estado de São Paulo; 2015.
- 17 Ministério da Saúde (BR), Fundação Nacional da Saúde. Manual de Instruções para o preenchimento da declaração de óbito. 3. ed. Brasília, DF: FUNASA; 2001.
-
18 Antunes JLF, Cardoso MRA. Uso da análise de séries temporais em estudos epidemiológicos. Epidemiol Serv Saude. 2015;24(3):565-76. https://doi.org/10.5123/S1679-49742015000300024
» https://doi.org/10.5123/S1679-49742015000300024 -
19 Ly KN, Xing J, Klevens RM, Jiles RB, Ward JW, Holmberg SD. The increasing burden of mortality from viral hepatitis in the United States between 1999 and 2007. Ann Intern Med. 2012;156(4):271-8. https://doi.org/10.7326/0003-4819-156-4-201202210-00004
» https://doi.org/10.7326/0003-4819-156-4-201202210-00004 -
20 Chang MH, Chen CJ, Lai MS, Hsu HM, Wu TC, Kong MS, et al. Universal hepatitis B vaccination in Taiwan and the incidence of hepatocellular carcinoma in children. N Engl J Med. 1997;336(26):1855-9. https://doi.org/10.1056/NEJM19970626336260
» https://doi.org/10.1056/NEJM19970626336260 -
21 Ni YH, Chang MH, Huang LM, Chen HL, Hsu HY, Chiu TY, et al. Hepatitis B virus infection in children and adolescents in a hyperendemic area: 15 years after mass hepatitis B vaccination. Ann Intern Med. 2001;135(9):796-800. https://doi.org/10.7326/0003-4819-135-9-200111060-00009
» https://doi.org/10.7326/0003-4819-135-9-200111060-00009 -
22 Grirnsven GJ, Vroome EM, Goudsmit J, Coutinho RA. Changes in sexual behavior and the fall in incidence of HIV infection among homosexual men. BMJ. 1989;298(6668):218-21. https://doi.org/10.1136/bmj.298.6668.218
» https://doi.org/10.1136/bmj.298.6668.218 -
23 Alter MJ, Hadler SC, Margolis HS, Alexander J, Hu PY, Judson FN, et al. The changing epidemiology of hepatitis b in the United States. Needs for alternative vaccination strategies. JAMA. 1990;263(9):1218-22. https://doi.org/10.1001/jama.1990.03440090052025
» https://doi.org/10.1001/jama.1990.03440090052025 -
24 Marotta P, Hueppe D, Zehnter E, Kwo P, Jacobson I. Efficacy of chronic hepatitis C therapy in community-based trials. Clin Gastroenterol Hepatol. 2009;7(10):1028-36. https://doi.org/10.1016/j.cgh.2009.05.003
» https://doi.org/10.1016/j.cgh.2009.05.003 -
25 Hansen N, Obel N, Christensen PB, Kjaer M, Laursen AL, Krarup HB, et al. Effectiveness of treatment with pegylated interferon and ribavirin in an unselected population of patients with chronic hepatitis C: a Danish nationwide cohort study. BMC Infect Dis. 2011;11:177. https://doi.org/10.1186/1471-2334-11-177
» https://doi.org/10.1186/1471-2334-11-177 -
26 Ford N, Kirby C, Singh K, Mills EJ, Cooke G, Kamarulzaman A, et al. Chronic hepatitis C treatment outcomes in low- and middle-income countries: a systematic review and meta-analysis. Bull World Health Organ. 2012;90(7):540-50. https://doi.org/10.2471/BLT.11.097147
» https://doi.org/10.2471/BLT.11.097147 - 27 Ministério da Saúde (BR), Secretaria de Vigilância em Saúde. Departamento de DST, Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para Hepatite C e coinfecções. Brasília, DF; 2015.
-
28 Razavi H, Elkhoury AC, Elbasha E, Estes C, Pasini K, Poynard T, et al. Chronic hepatitis C virus (HCV) disease burden and cost in the United States. Hepatology 2013;57(6):2164-70. https://doi.org/10.1002/hep.26218
» https://doi.org/10.1002/hep.26218 -
29 Mahajan R, Xing J, Liu SJ, LyKN, Moorman AC, Rupp L, et al. Mortality among persons in care with hepatitis C virus infection: the Chronic Hepatitis Cohort Study (CheCS), 2006–2010. Clin Infect Dis. 2014;58(8):1055-61 https://doi.org/10.1093/cid/ciu077
» https://doi.org/10.1093/cid/ciu077 -
30 Pinchoff J, Drobnik A, Bornschlegel K, Braunstein S, Chan C, Varma JK et al. Deaths among people with hepatitis C in New York City, 2000-2011. Clin Infect Dis. 2014;58(8):1047-54. https://doi.org/10.1093/cid/ciu075
» https://doi.org/10.1093/cid/ciu075 - 31 Ministério da Saúde (BR), Agência Nacional de Vigilância Sanitária. Portaria Nº 4, de 7 de fevereiro de 1986. Normaliza o uso e reutilização de materiais médico-hospitalares descartáveis no país. Diário Oficial União. 12 fev 1986;(28).
-
32 Ly KN, Xing J, Klevens RM, Jiles RB, Holmberg SD. Causes of death and characteristics of decedents with viral hepatitis, United States, 2010. Clin Infect Dis 2014;58(1):40-9. https://doi.org/10.1093/cid/cit642
» https://doi.org/10.1093/cid/cit642 -
33 Perz JF, Armstrong GL, Farrington LA, Hutin YJF, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol. 2006;45(4):529-38. https://doi.org/10.1016/j.jhep.2006.05.013
» https://doi.org/10.1016/j.jhep.2006.05.013 -
34 Sulkowski MS. Viral hepatitis and HIV coinfection. J Hepatol. 2008;48(2):353-67. https://doi.org/10.1016/j.jhep.2007.11.009
» https://doi.org/10.1016/j.jhep.2007.11.009 -
35 Walter SR, Thein HH, Amin J, Gidding HF, Ward K, Law MG, et al. Trends in mortality after diagnosis of hepatitis B or C infection: 1992-2006. J Hepatol. 2011;54(5):879-86. https://doi.org/10.1016/j.jhep.2010.08.035
» https://doi.org/10.1016/j.jhep.2010.08.035 -
36 Lédinghen V, Barreiro P, Foucher J, Labarga P, Castéra L, Vispo ME, et al. Liver fibrosis on account of chronic hepatitis C is more severe in HIV-positive than HIV-negative patients despite antiretroviral therapy. J Viral Hepat. 2008;15(6):427-33. https://doi.org/10.1111/j.1365-2893.2007.00962.x
» https://doi.org/10.1111/j.1365-2893.2007.00962.x -
37 Redelings MD, Sorvillo F, Simon P. A comparison of underlying cause and multiple causes of death. Epidemiology. 2006;17(1):100-3. https://doi.org/10.1097/01.ede.0000187177.96138.c6
» https://doi.org/10.1097/01.ede.0000187177.96138.c6 -
38 Oliveira BZ, Gotlieb SLD, Laurenti R, Mello Jorge MHP. Mortalidade feminina por hipertensão: análise por causas múltiplas. Rev Bras Epidemiol. 2009;12(4):556-65. https://doi.og/10.1590/S1415-790X2009000400006
» https://doi.og/10.1590/S1415-790X2009000400006 - 39 Ministério da Saúde (BR), Secretaria de Vigilância em Saúde. Departamento de Vigilância, Prevenção e Controle das Infecções Sexualmente Transmissíveis, do HIV/Aids e das Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para Hepatite C e coinfecções; Brasília, DF; 2019.
-
40 Kabiri M, Jazwinski AB, Roberts MS, Schaefer AJ, Chhatwal J. The changing burden of hepatitis C virus infection in the United States: model-based predictions. Ann Intern Med. 2014;161(3):170-80. https://doi.org/10.7326/M14-0095
» https://doi.org/10.7326/M14-0095
Publication Dates
-
Publication in this collection
04 Dec 2020 -
Date of issue
2020
History
-
Received
28 Nov 2019 -
Accepted
18 Mar 2020

 Mortality trend due to Hepatitis B and C in the city of São Paulo, 2002–2016
Mortality trend due to Hepatitis B and C in the city of São Paulo, 2002–2016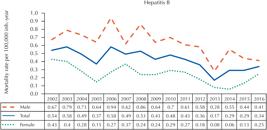


 Source: SIM/PRO-AIM/CEINFO/SMSSP.
Source: SIM/PRO-AIM/CEINFO/SMSSP.
 Source: SIM/PRO-AIM/CEINFO/SMSSP.
Source: SIM/PRO-AIM/CEINFO/SMSSP.