ABSTRACT
OBJECTIVE Describe the profile of hospitalizations for cancer diagnosis in Brazil from 2008 to 2018 at Unified Health System (SUS).
METHODS Time series study of hospitalization rate for malignant neoplasms at SUS. Data were extracted from the Hospital Information System of DataSUS. The trend was estimated using generalized linear regression, applying the Prais-Winsten estimation procedure.
RESULTS From 2008 to 2018, the hospitalization rate for malignant neoplasms showed an increasing trend at SUS, with an annual variation of 10.7% (p < 0.001; CI = 9.4–11.7). An increasing trend of hospitalizations in all regions of Brazil was observed, except in the Northern region, which remained unchanged. The Northeastern region presented the highest annual variation (13.5%; p < 0.001), whereas the Southern and Southeastern regions had the highest hospitalization rates per 100,000 inhabitants, resulting in 506 and 325 hospitalizations, respectively. We observed a significant increasing trend in hospitalizations of children aged 0 to 9 years (annual variation = 10.9%; p < 0.001); young people, 10 and 19 years (annual variation = 6.9%; p < 0.001); and older adults; over 60 years (annual variation = 7.9%; p < 0.001). Among women, hospitalizations occurred mainly due to malignant neoplasm of the breast (annual variation = 13.2%; p < 0.001); and among men, malignant neoplasm of the prostate (annual variation = 4.7%; p < 0.001).
CONCLUSION Hospitalizations for malignant neoplasms showed an increasing trend, in line with the increased incidence of cancer, in particular, the most frequent neoplasms between men and women. Although the Northeastern region showed the highest variation in the period, the Southern and Southeastern regions had the highest hospitalization rates in the country. We also observed an increase in hospitalizations among the young (between 0 and 19 years old) and older adults (over 60 years) population. Hospitalizations for neoplasm of the cervix in women, although still the third cause of hospitalizations, showed decreasing behavior.
Neoplasms; Hospitalization, trends; Access to Health Services, trends; Differences in Health Care; Time-series studies
RESUMO
OBJETIVO Descrever o perfil das internações pelo Sistema Único de Saúde (SUS) por diagnóstico de câncer no Brasil no período de 2008 a 2018.
MÉTODOS Estudo de séries temporais da taxa de internação por neoplasias malignas no SUS. Os dados foram extraídos do Sistema de Informações Hospitalares do DataSUS. A tendência foi estimada por regressão linear generalizada, aplicando o procedimento de Prais-Winsten.
RESULTADOS No período de 2008 a 2018, a taxa de internação por neoplasias malignas apresentou tendência crescente no SUS, com variação anual de 10,7% (p < 0,001; IC = 9,4–11,7). Observou-se tendência crescente de internações em todas as regiões do Brasil, com exceção da região Norte, que apresentou comportamento estacionário. A região Nordeste foi a que apresentou maior variação anual (13,5%; p < 0,001), enquanto as regiões Sul e Sudeste apresentaram as maiores taxas de internação por 100 mil habitantes, 506 e 325 respectivamente. Observou-se tendência crescente significativa nas internações de crianças de 0 a 9 anos de idade (variação anual = 10,9%; p < 0,001), de jovens entre 10 e 19 anos (variação anual = 6,9%; p < 0,001) e de idosos acima de 60 anos (variação anual = 7,9%; p < 0,001). Entre as mulheres, as internações ocorreram majoritariamente por neoplasia maligna de mama (variação anual = 13,2%; p < 0,001), e entre os homens por neoplasia maligna de próstata (variação anual = 4,7%; p < 0,001).
CONCLUSÃO As internações por neoplasias malignas mostraram tendência crescente, em consonância com o aumento da incidência de câncer, em particular das neoplasias mais incidentes entre homens e mulheres. Apesar da região Nordeste ter apresentado maior variação no período, as regiões Sul e Sudeste apresentaram as maiores taxas de internação do país. Observou-se também aumento das internações entre a população jovem (entre 0 e 19 anos) e mais idosa (acima de 60 anos). As internações por neoplasias de colo de útero nas mulheres, embora ainda sejam a terceira causa de internações, apresentaram comportamento decrescente.
Neoplasias; Hospitalização, tendências; Acesso aos Serviços de Saúde, tendências; Disparidades em Assistência à Saúde; Estudos de Séries Temporais
INTRODUCTION
Together with cardiovascular, and respiratory diseases and diabetes, cancer is part of the set of chronic non-communicable diseases (NCDs) that cause the most deaths in the world. Cancer reaches individuals in all age groups. When it reaches the economically active young populations1, it leads them to disabilities. Currently, cancer ranks second in the ranking of mortality due to NCDs, with an incidence of 24.3 million new cases worldwide in 20172,3.
In biennium 2014–2015, an incidence of 576,000 new cases of cancer per year was estimated in Brazil. Incidences of more than 600,000 and 625,000 new cases of cancer were predicted to occur for the biennium 2018–2019 and 2020–2021, respectively2,4,5.
The Unified Health System (SUS), created by Law No. 8,080/1990, ensures universal access to health services at all levels of care and completeness of care in Brazil6. To ensure these principles in cancer treatment, Ordinance No. 874 was published in 2013 and established the National Policy for Cancer Prevention and Control in the Health Care Network of People with Chronic Diseases. The establishment of this ordinance aims to reduce mortality and disabilities caused by cancer, and the incidence of some types of cancer by diagnosing early and using screening programs7.
Ordinance No. 874 also establishes the criteria for guidance for patients to access health services. In December 2019, the specialized outpatient and hospital care network in oncology at SUS covered 419 services qualified in high oncologic complexity, 9 isolated radiotherapy services, and 21 general hospitals with oncologic surgery8. We highlight that clinical hospitalizations also occur in other SUS services.
Clinical treatments, which include chemotherapy and radiotherapy performed on an outpatient basis, are recorded by High Complexity Procedure Authorizations (APAC) and represent the highest percentage of procedures related to cancer treatment in the country. Surgical hospitalizations of cancer patients occur so the performance of biopsies and surgical treatment be done, whereas clinical hospitalizations occur for continuous infusion chemotherapy or the treatment of cancer complications, as in cases of clinical decompensation requiring hospitalization support. The latter can occur in any type of hospital, and not only in specialized ones9.
Cancer treatment presents a high cost compared to the other treatments offered by SUS. A study conducted by Barros Reis10 showed that the average cost of cancer treatment in Brazil was around US$ 3,796.00 per patient in 2011, and 30% are related to hospitalizations; and the rest, outpatient procedures. In a survey on costs of cervical cancer treatment in public services in 2006, Novaes et al.11 observed that, of US$ 104,966,045, about 8% were destined for clinical hospitalizations. In a recent study, we observed that the costs of hospitalizations of patients with cervical cancer reached 22.2%12.
Evidence suggests that hospitalizations for malignant neoplasms have an important role in cancer treatment and, therefore, studying this theme is relevant. Studying how hospitalizations are managed helps to understand the spatial distribution of these treatments at SUS, identifying whether there is a concentration of hospitalizations or health care voids in the regions of the country. Considering this background, this study analyzes trends and describes the profile of hospitalizations for cancer diagnosis at SUS, in Brazil, between 2008 and 2018.
METHODS
This is a descriptive time series study conducted using data from the Sistema de Informação Hospitalar (Hospital Information System - SIH) of the SUS Department of Informatics (DATASUS). Data were divided into geographic regions, and frequencies were adjusted for the resident population to obtain the appropriate proportion of individuals in each analyzed group13,14.
The SIH, established by Ordinance No. 896/1990 of the Ministry of Health, adopts the Hospital Admission Authorization as an instrument to be used by all public administrators and service providers of the SUS to record and process patient identification data, procedures performed, health professionals involved and hotel structure15.
In this study, data extracted from SIH were tabulated in the TabWin program version 4.1.5. The national tables and definition files were obtained from the DataSUS website (http://www2.datasus.gov.br/DATASUS/index.php). The data, extracted in January 2020 and aggregated by year, refer to hospitalizations for malignant neoplasms that occurred in health facilities that were attended by the SUS from January 2008 to December 2018. While this study focuses on hospitalizations for malignant neoplasms, only hospitalizations corresponding to codes C00-C97 were considered, according to Chapter II of the 10th International Classification of Diseases (ICD).
We should highlight that the same patient may have undergone several hospitalizations during the analysis period and that not all cancer patients undergo any hospitalization at SUS. Thus, the proportion of deaths cannot be considered as a mortality rate of hospitalizations, nor as a mortality rate due to cancer at SUS, since not all patients progress to death during hospitalization.
The population data we provided by the Brazilian Institute of Geography and Statistics (IBGE) and were consulted in the statistical table database of the institute (https://sidra.ibge.gov.br/home/pms/brasil).
For the Brazil level, the hospitalization rate was calculated as the ratio among the total number of hospitalizations by the total annual population. For the analysis stratified by complexity (medium and high complexity), type of hospitalization (elective and urgent), the outcome of hospitalization (discharge and death), length of stay, and ICU stay, the ratio was considered between the number of hospitalizations in each stratum and the total population for each year. For sex, age group, and state, the ratio between the hospitalization rate and the population in the same stratum per year was calculated (for example, the incidence rate for females is the ratio between the number of hospitalizations of women and the annual Brazilian female population). Incidence rates were adjusted per 100,000 inhabitants. In the analysis of hospitalizations by ICD codes stratified by sex, only the 20 most frequent ICD codes were considered in 2018 for each sex.
To analyze the trend of the standardized hospitalization rate, the methodology of time series analysis described by Antunes and Cardoso14was applied, and the following trend model was estimated for the decade of 2008 to 2018:
Where taxat is the rate of hospitalization for malignant neoplasms in the year t and u is the error of the regression. The coefficient β1 indicates the trend of the time series, so that the estimated value represents the change in log(taxat) for each additional year t. Thus, if the coefficient β1 is positive, the trend of the series is increasing and, if it is negative, the trend is decreasing. The rate transformation allows the trend to be expressed in percentage terms and aims to normalize the distribution and stabilize variance, which is one of the assumptions of the model.
The model was estimated using a generalized linear regression model, applying the Prais-Winsten estimation with robust variance. The method is indicated to adjust the existing serial autocorrelation in time-series analyses to heteroscedasticity and obtain robust statistics. From the robust variance, the appropriate confidence interval and p-value for statistical inference were calculated.
To obtain the trend of the series measured by the average annual variation (VMA) in percentage terms, the following formula was applied14:
The VMA confidence interval was calculated similarly using the minimum (β1min) and maximum (β1max) values obtained from the estimation of the trend model14:
Finally, we reported whether the estimated annual mean variation was unchanged (p > 0.05), decreasing (p < 0.05 and negative variation) or increasing (p < 0.05 and positive variation) in each stratum evaluated14.
The data were analyzed in the statistical program Stata, version 16. Because this study avails itself of secondary data from the public domain, submitting the project for analysis by the Research Ethics Committee was not necessary, according to Resolution of the National Health Council No. 466/201216.
RESULTS
From January 2008 to December 2018, there were 5,469,895 hospitalizations of patients diagnosed with malignant neoplasms, equivalent to 4.4% of all hospitalizations by SUS in the same period. Regarding the total number of hospitalizations for cancer, 51.8% were female, 79.7% were patients over 40 years of age, and 43.4% were hospitalizations of high complexity. Concerning the type of hospitalization, 51.4% were elective, and 10.2% died. Regarding the length of stay, 50.9% of hospitalizations were up to 3 days, 20.2% between 4 and 6 days, 11.5% between 7 and 9 days, and the others above 10 days of hospitalization (17.2%).
Figure 1 shows the estimated and observed hospitalization rates by region. The Southern region had the highest rate of hospitalizations in the country, with an average of 391 hospitalizations per 100,000 inhabitants per year, followed by the Southeastern (277 per 100,000 inhabitants), Midwestern (211), Northeastern (188), and Northern (97) regions.
Time series of the rate of hospitalization observed (points) and estimated (line)a for malignant neoplasms (number of hospitalizations per 100,000 inhabitants), per region. Brazil, 2008 to 2018.
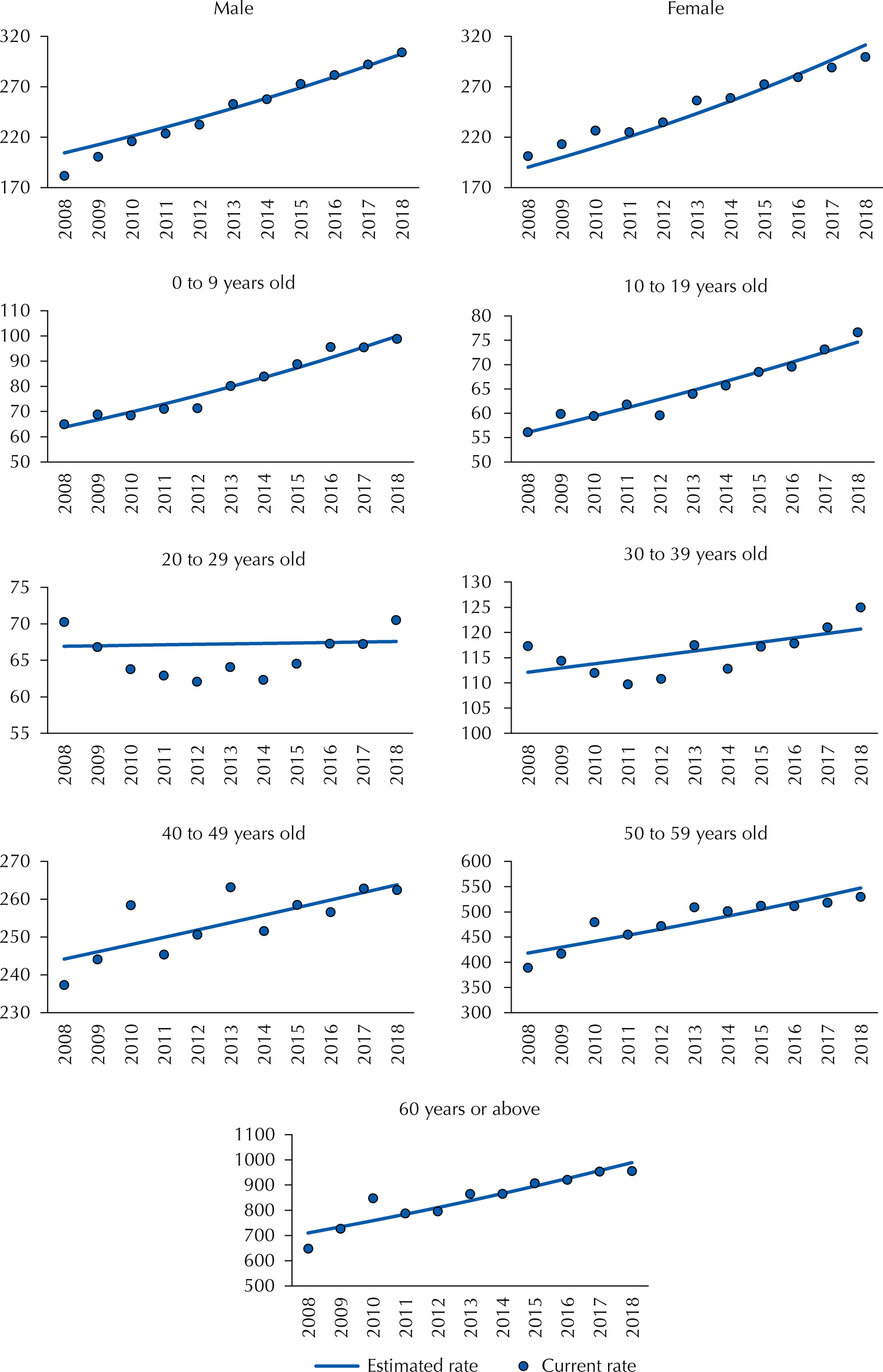
Figure 2 shows the hospitalization rates observed and estimated by the trend model, according to the population’s demographic profile (sex and age). Figures 1 and 2 together indicate that the actual historical series of the hospitalization rate has a behavior close to that of the series estimated by the linear trend model.
Time series of the rate of hospitalization observed (points) and estimated (line)a for malignant neoplasms (number of hospitalizations per 100,000 inhabitants), by demographic profile. Brazil, 2008 to 2018.
Tables 1 to 3 show the results of the trend analysis for the period 2008 to 2018 and the values of hospitalization rates for malignant neoplasms observed in the initial period (2008) and the final period (2018) of the historical series studied.
Table 1 presents the trend analysis of hospitalizations by region and state. In Brazil, the trend was increasing, with an average annual variation of 10.7% (p < 0.000). An increasing trend in the Northeast (annual variation = 13.5%; p < 0.001), Southeast (annual variation = 10.4%; p < 0.001), South (13.2%; p < 0.001) and Midwest (3.5%, p = 0.043) was observed. Only the Northern region showed an unchanged trend, with an annual change of 2.8% (p = 0.115).
In 2008, Tocantins had the highest hospitalization rate in the North, but over the years, this rate decreased 6% per year (p = 0.023), while Rondônia and Amapá showed an increasing trend, with annual variations of 60.7% (p < 0.001) and 2.3% (p < 0.001) respectively.
The Northeastern region showed the largest annual percentage change among the five Brazilian regions. Only Sergipe and Piauí showed an unchanged trend within all the states of the region, with annual variations of 1.2% (p = 0.257) and 3% (p = 0.307). Paraíba (annual variation = 23.9%, p < 0.001), Pernambuco (annual variation = 21.6%, p < 0.001), Alagoas (annual variation = 18.9%, p < 0.001) and Rio Grande do Norte (annual variation = 18.6%, p < 0.001) had the most significant mean annual variations observed in the region.
Table 2 shows the rate of hospitalization per profile of patients. Both men and women, the trend was increasing, with annual variations of 11.9% (p < 0.001) and 9.4% (p < 0.001) respectively. We also observed an increasing trend in the age groups from 0 to 9 years (annual variation = 10.9%, p < 0.001), from 10 to 19 years (annual variation = 6.9%, p < 0.001), 40 to 49 years (annual variation = 1.9%; p = 0.001), 50 to 59 years (annual change = 6.4%; p = 0.001) and over 60 years (annual variation = 7.9%; p < 0.001). In the age groups between 20 and 39 years, the trend was unchanged. The other groups analyzed showed increasing trends, except for the permanence above 25 days, which was unchanged. No decreasing trend in the analyzed profile in any of the groups studied was observed.
High complexity hospitalizations presented an annual variation of 17.8% per year (p = 0.001). This fact may be related to the increase in the rate of hospitalizations in which patients needed ICU (15.1% per year, p < 0.001). This data suggest an increase in hospitalizations for surgical purposes when associated with the fact that hospitalizations with a length of stay of up to three days varied by 15.9% per year (p = 0.001).
Table 3 represents the trends of hospitalization for malignant neoplasms in females and males for the 20 ICD codes with the highest hospitalization rates in 2018 for each sex.
Among women, the most frequent hospitalization rates showed increasing behavior, with significant annual variation. Hospitalizations for malignant breast cancer went from 36.4 per 100,000 women in 2008 to 62.6 per 100,000 women in 2018, with a growth trend of 13.2% per year (p < 0.001). Then, the most frequent hospitalizations in 2018 were for malignant neoplasms of the colon, with 23.1 per 100,000 women (annual variation = 19.1%; p < 0.001), cervix, with 20.5 per 100,000 women (annual variation = −4.7%; p = 0.011), other malignant skin neoplasms, with 19.6 per 100,000 women (annual variation = 27.9%; p < 0.001), and ovary, with 11.1 per 100,000 women (annual variation = 12.5%; p < 0.001).
In men, we observed an increasing trend in the rate of hospitalizations for the main ICD codes. In this group, the main causes of hospitalization were malignant neoplasms of the prostate, with 32.1 per 100,000 men (annual variation = 4.7%, p = 0.001), followed by malignant neoplasms of the colon , with 24 per 100,000 men (annual variation = 19.1%; p < 0.001), other malignant neoplasms of the skin, with 22.4 per 100,000 men (17.2%; p < 0.001), stomach, with 19 per 100,000 men (annual variation = 14%; p < 0.001), and malignant neoplasm of the esophagus, with 14 per 100,000 men (annual variation = 7.9%; p = 0.025).
DISCUSSION
The analyzed database represents hospitalizations for malignant neoplasms attended by SUS. The frequency of 50.9% of hospitalizations of up to three days refers to surgical hospitalizations or for continuous administration chemotherapy. Longer hospitalizations are usually related to clinical or surgical complications.
Hospitalizations for malignant neoplasms tended to have a significant increase in the country over the period analyzed, with an annual variation of 10.7%. The Northeastern region experienced the largest annual proportional increase in hospitalizations (13.5%), followed by the Southern (13.2%) and Southeastern regions (8.6%). However, the Southern and Southeastern regions had the highest hospitalization rates in 2018, 506 and 325 per 100,000 inhabitants, respectively. These regions have greater availability of services, which increases access to diagnosis, treatment, and hospitalization17. For comparison purposes, among 449 establishments qualified in some specialized oncology service, 102 (23%) are located in the South; and 220 (49%), in the Southeast. On the other hand, the lack of care in oncology in the North and Northeast leads patients to seek specialized services in the most assisted regions18.
The increase in hospitalizations among children and young people up to 19 years of age should be observed, since, because it occurs less in this age group, there is a lower supply of specialized services for this public. A study by Grabois et al. demonstrated the need to travel long distances so that young people and children receive adequate care18. This factor concentrates patients in certain locations, increasing the rate of hospitalizations or treatments in specific regions.
Planning the appropriate distribution of reference centers is important, considering that these are events with lower incidence rates and, therefore, the services will not be made available as often as those related to the most incident neoplasms, even to ensure qualified and specialized care for younger people. For this purpose, health care networks must work in an interconnected way, to direct the patient to the service that offers the indicated treatment.
A study on hospitalizations of children and adolescents with neoplasms in Ribeirão Preto (SP) showed that there are patients from the five regions of the country assisted in the city, which is a reference site for the treatment of onco-hematological diseases with services and specialized staff19. The study shows that this concentration of services can interfere with treatment since patients do not always return with adequate frequency due to distance or financial difficulties19.
In the study, the highest hospitalization rate among women occurred due to malignant breast cancer, followed by colon neoplasm, corroborating to national estimates that show breast cancer as the most frequent among the female population2,4,20.
There is a decreasing trend of hospitalizations due to malignant neoplasms of the cervix. This decline may be the result of the implementation of prevention policies and early diagnosis for this type of cancer. A Study by Arbyn et al.21 on cervical cancer demonstrates a global fall in the incidence of this neoplasm, except for some regions in Africa, since there is still difficulty in accessing preventive measures and early diagnosis in less developed regions22.
Among men, hospitalizations for malignant neoplasm of the prostate were the most frequent, followed by colon, corroborating national estimates. Malignant neoplasms of the prostate are closely related to age. It is a type of cancer that usually develops slowly, with symptoms that basically affect the genitourinary system and usually lead to hospitalizations2,4,20,23.
As for lung cancer, one of the most lethal nowadays, it should be noted that it presented low hospitalization rates among both men and women. This type of cancer, when diagnosed in the early stages, can be surgically resected, but its diagnosis usually occurs in late stages, when only clinical treatments (chemotherapy and radiotherapy) are possible24,25, which leads to hospitalizations only in cases of clinical decompensation.
The ICD code of other skin neoplasms appeared as the third cause of hospitalizations among men and the fourth among women. Studies conducted locally already pointed to this occurrence. Most neoplasms that affect the skin are treated at the outpatient level, even when they require surgical treatments. The importance of hospitalization rates due to skin neoplasms draws attention to the fact that life habits, such as protection against ultraviolet radiation, are fundamental to prevent the occurrence of this type of cancer. These data point out the need for prevention programs aimed at sensitizing the population on the subject26,27.
The study aimed to outline the profile of hospitalizations due to cancer in patients attended by SUS. We observed that hospitalization rates for cancer increased significantly in the period studied. Data from the Northeastern region, with the highest annual average variation, and the Southern and Southeastern regions, with the highest rates of hospitalization for malignant neoplasms in the country and the highest concentration of specialized resources provided by the SUS. Hospitalizations in age groups below 19 years and above 60 years showed a significant increasing trend in the period. Hospitalizations for malignant neoplasms of the breast were, in isolation, the main cause of hospitalization for cancer among women, whereas malignant neoplasms of the prostate also, in isolation, took the centre stage in hospitalization rate among men.
An important point observed in this study is the existence of health care voids in the most deprived regions, which forces patients to move to distant and specialized centers, often located in other states. It is noteworthy the need for further studies on this subject to be carried out.
Among the limitations of the research, it is worth noting that, as the data represent the number of hospitalizations, it is not possible to infer from them the incidence or mortality rates due to cancer. Not all patients diagnosed with malignant neoplasm are hospitalized, and the same patient may require more than one hospitalization per year, depending on the clinical picture and the evolution of the disease. It is also necessary to consider the cases of neoplasm treated in private care, whose information is not available in the database studied. In addition, it should be considered the fact that the oncological clinical treatment performed through chemotherapy and radiotherapy is processed by the Outpatient Information System (SIA), which was not used in this study.
Another limitation of this study is the absence of analysis of the interactions between the various subgroups analyzed. An example: although the trend for the age group from 20 to 29 years is unchanged, the behavior of the series may be different for men and women in the same subgroup.
Because this is a research conducted with secondary data, there could be a certain limit regarding the reliability of the data presented due to discrepancies in the collection of information or the registration in the SUS systems. However, the Hospital Information System is the official database of the Ministry of Health, and its data support the planning of care and the formulation or adequacy of public policies. Thus, despite possible limitations, the analyzed data can be considered valid.
REFERENCES
- 1 World Health Organization. Global Status Report on Noncommunicable Diseases 2014. Geneva (CH); WHO; 2014.
- 2 Instituto Nacional de Câncer José Alencar Gomes da Silva. Estimativa 2018: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2017.
-
3 GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(101590:1789-858. https://doi.org/10.1016/S0140-6736(18)32279-7
» https://doi.org/10.1016/S0140-6736(18)32279-7 - 4 Instituto Nacional de Câncer José Alencar Gomes da Silva. Estimativa 2014: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2014.
- 5 Instituto Nacional de Câncer José Alencar Gomes da Silva. Estimativa 2020: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2019.
- 6 Brasil. Lei Nº 8.080, de 19 de setembro de 1990. Lei Orgânica da Saúde. Dispõe sobre as condições para a promoção, proteção e recuperação da saúde, a organização e o funcionamento dos serviços correspondentes e dá outras providências. Diário Oficial da União. 20 set 1990; Seção 1:18055.
-
7 Ministério da Saúde (BR). Portaria Consolidação Nº 2, de 28 de setembro de 2017. Consolidação das normas sobre as políticas de saúde do Sistema Único de Saúde. Anexo IX - Institui a Política Nacional para a Prevenção e Controle do Câncer na Rede de Atenção à Saúde das Pessoas com Doenças Crônicas no âmbito do SUS. Brasília, DF; 2017 [cited 2020 Feb 5]. Available from: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2017/prc0002_03_10_2017.html
» https://bvsms.saude.gov.br/bvs/saudelegis/gm/2017/prc0002_03_10_2017.html -
8 Ministério da Saúde (BR), Departamento de Informática do SUS. Tabnet: Informações de Saúde. CNES – estabelecimentos por habilitação - Brasil. Brasília, DF; 2020 [cited 2020 Feb 5]. Available from: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?cnes/cnv/habbr.def
» http://tabnet.datasus.gov.br/cgi/tabcgi.exe?cnes/cnv/habbr.def -
9 Ministério da Saúde (BR), Secretaria de Atenção à Saúde, Departamento de Regulação, Avaliação e Controle, Coordenação Geral de Sistemas de Informação. SIA/SUS - Sistema de Informações Ambulatoriais. Manual de bases técnicas da oncologia. 25. ed. Brasilia, DF; 2019 [cited 2020 Feb 5]. Available from: http://sbradioterapia.com.br/wp-content/uploads/2019/05/Manual-Oncologia_25a_edicao.pdf
» http://sbradioterapia.com.br/wp-content/uploads/2019/05/Manual-Oncologia_25a_edicao.pdf -
10 Reis CB, Knust RE, Pereira CCA, Portela MC. Factors associated with non-small cell lung cancer treatment costs in a Brazilian public hospital. BMC Health Serv Res. 2018;18:124. https://doi.org/10.1186/s12913-018-2933-0
» https://doi.org/10.1186/s12913-018-2933-0 -
11 Novaes HMD, Itria A, Silva GA, Sartori AMC, Rama CH, Soárez PC. Annual national direct and indirect cost estimates of the prevention and treatment of cervical cancer in Brazil. Clinics (Sao Paulo). 2015;70(4):289-95. https://doi.org/10.6061/clinics/2015(04)12
» https://doi.org/10.6061/clinics/2015(04)12 -
12 Santos CL, Souza AI, Figueiroa JN, Vidal SA. Estimation of the costs of invasive cervical cancer treatment in Brazil: a micro-costing study. Rev Bras Ginecol Obstet. 2019;41(6):387-93. https://doi.org/10.1055/s-0039-1692412
» https://doi.org/10.1055/s-0039-1692412 - 13 Pereira MG. Epidemiologia: teoria e prática, Rio de Janeiro: Guanabara Koogan; 2015. Estudos Descritivos; p. 271-2.
-
14 Antunes JLF, Cardoso MRA. Uso da análise de séries temporais em estudos epidemiológicos. Epidemiol Serv Saude. 2015;24(3):565-76. https://doi.org/10.5123/S1679-49742015000300024
» https://doi.org/10.5123/S1679-49742015000300024 - 15 Ministério da Saúde (BR). SIH – Sistema de Informação Hospitalar do SUS: manual técnico operacional do Sistema. Brasília, DF; 2017.
-
16 Conselho Nacional de Saúde (BR). Resolução Nº 466, de 12 de dezembro de 2012. Resolve aprovar as diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos. Brasília, DF: CNS; 2012 [cited 2020 Feb 5]. Available from: https://conselho.saude.gov.br/resolucoes/2012/Reso466.pdf
» https://conselho.saude.gov.br/resolucoes/2012/Reso466.pdf -
17 Oliveira MM, Malta DC, Guauche H, Moura L, Silva GA. Estimativa de pessoas com diagnóstico de câncer no Brasil: dados da Pesquisa Nacional de Saúde, 2013. Rev Bras Epidemiol. 2015;18 Supl 2:144-57. https://doi.org/10.1590/1980-5497201500060013
» https://doi.org/10.1590/1980-5497201500060013 -
18 Grabois MF, Oliveira EXG, Carvalho MS. Assistência ao câncer entre crianças e adolescentes: mapeamento dos fluxos origem-destino no Brasil. Rev Saude Publica. 2013;47(2):368-78. https://doi.org/10.1590/s0034-8910.2013047004305
» https://doi.org/10.1590/s0034-8910.2013047004305 -
19 Pan R, Marques AR, Costa Júnior MLC, Nascimento LC. Characterization of the hospitalization of children and adolescents with cancer. Rev Lat Am Enfermagem. 2011;19(6):1413-20. https://doi.org/10.1590/s0104-11692011000600019
» https://doi.org/10.1590/s0104-11692011000600019 - 20 Instituto Nacional de Câncer José Alencar Gomes da Silva. Estimativa 2016: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2015.
-
21 Arbyn M, Weiderpass E, Bruni L, Sanjosé S, Saraiya M, Ferlay J, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8(2):e191-203. https://doi.org/10.1016/S2214-109X(19)30482-6
» https://doi.org/10.1016/S2214-109X(19)30482-6 -
22 Tsuchiya CT, Lawrence T, Klen MS, Fernandes RA, Alves MR. O câncer de colo do útero no Brasil: uma retrospectiva sobre as políticas públicas voltadas à saúde da mulher. J Bras Econ Saude. 2017;9(1):137-47. https://doi.org/10.21115/jbes.v9.n1.p137-47
» https://doi.org/10.21115/jbes.v9.n1.p137-47 -
23 Gnanaraj J, Balakrishnan S, Umar Z, Antonarakis ES, Pavlovich CP, Wright SM, et al. Medical hospitalizations in prostate cancer survivors. Med Oncol. 2016;33(7):81. https://doi.org/10.1007/s12032-016-0796-y
» https://doi.org/10.1007/s12032-016-0796-y -
24 Nasim F, Sabath BF, Eapen GA. Lung cancer. Med Clin North Am. 2019;103(3):463-73. https://doi.org/10.1016/j.mcna.2018.12.006
» https://doi.org/10.1016/j.mcna.2018.12.006 -
25 Algranti E, Menezes AMB, Achutti AC. Lung cancer in Brazil. Semin Oncol. 2001;28(2):143-52. https://doi.org/10.1016/s0093-7754(01)90085-5
» https://doi.org/10.1016/s0093-7754(01)90085-5 -
26 Dantas MM, Pires DAL, Schmitt DT, Nascimento VS, Turine CA. Estudo ecológico das internações por neoplasias malignas da pele na região norte no período de 2000 a 2014. Rev Cereus. 2016;8:23-40. https://doi.org/10.18605/2175-7275/cereus.v8n2p23-40
» https://doi.org/10.18605/2175-7275/cereus.v8n2p23-40 -
27 Guimarães RQ, Oliveira LCM, Calado VC, Barbosa RNF. Incidência de neoplasias malignas da pele no estado da Paraíba. Rev Saude Cienc Online. 2019;8:86-94. https://doi.org/10.35572/rsc.v8i2.46
» https://doi.org/10.35572/rsc.v8i2.46
Publication Dates
-
Publication in this collection
22 Nov 2021 -
Date of issue
2021
History
-
Received
28 Sept 2020 -
Accepted
16 Dec 2020

 Profile of hospitalizations for neoplasms in the Brazilian Unified Health System: a time-series study
Profile of hospitalizations for neoplasms in the Brazilian Unified Health System: a time-series study


 a Average annual percentage change of hospitalization rates calculated from the β 1 coefficient of the trend model estimated by generalized linear regression by the Prais-Winsten estimation13.
a Average annual percentage change of hospitalization rates calculated from the β 1 coefficient of the trend model estimated by generalized linear regression by the Prais-Winsten estimation13.
 a Average annual percentage change of hospitalization rates calculated from the β 1 coefficient of the trend model estimated by generalized linear regression by the Prais-Winsten estimation13.
a Average annual percentage change of hospitalization rates calculated from the β 1 coefficient of the trend model estimated by generalized linear regression by the Prais-Winsten estimation13.